Cervical cancer is one of the most common cancers among women globally, and the majority of deaths occur in low- and middle-income countries.
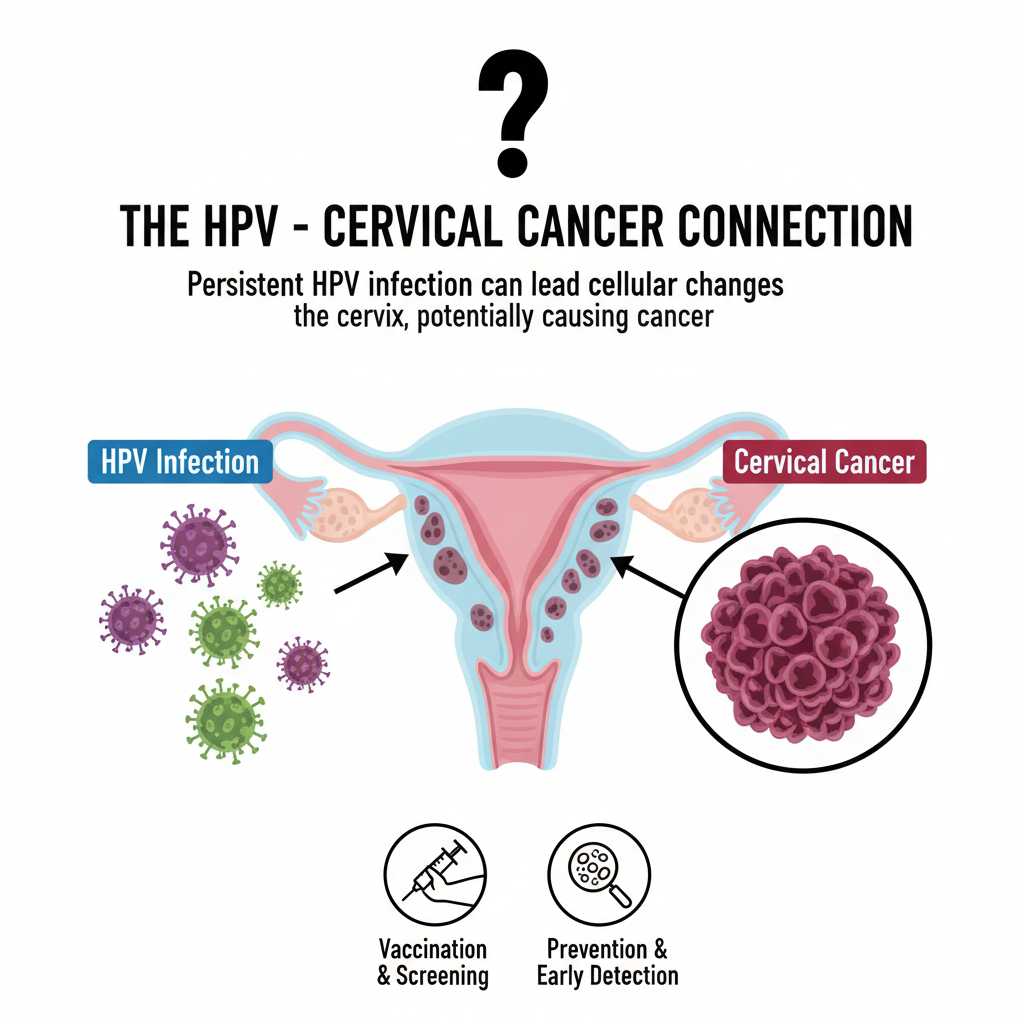
At the center of this illness is the human papillomavirus (HPV), an ordinary infection that, when persistent, can cause cancer of the cervix. It is important to understand the connection between HPV and cervical cancer for prevention, early detection, and treatment.
The truth is straightforward: although not all HPV infections develop into cancer, persistent infection with high-risk HPV is the main cause of most cervical cancers.
Because of this, prevention through vaccination and screening is one of the strongest weapons against women’s health today.
Table of Contents
ToggleWhat is HPV (Human Papillomavirus)?
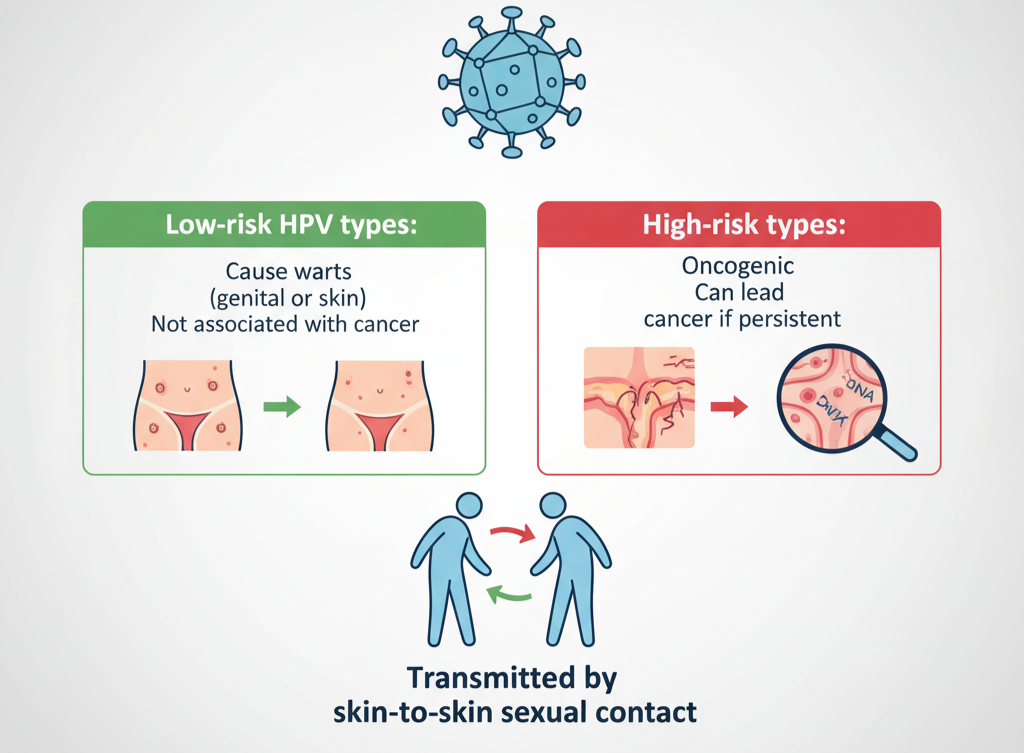
HPV, or human papillomavirus, is a family of over 200 related viruses. They are generally classified into:
Low-risk HPV types: These cause warts (genital or skin) but are not associated with cancer.
High-risk HPV types: Also referred to as oncogenic HPV, which has the ability to induce cellular changes that will lead to cancer if the infection is not cleared.
HPV is transmitted mainly by skin-to-skin sexual contact. It’s really, really common that HPV infection is most common and most people will be affected at the same time.
Most infections resolve on their own in 1–2 years, but when they don’t, the risk of cervical cancer grows.
How HPV leads Cervical Cancer
Development from HPV infection to cervical cancer is a multistep biological process:
Chronic infection is the most important risk factor. One exposure doesn’t typically lead to cancer; instead, it’s the chronic persistence of persistent high-risk types of HPV that leads to disease.
Viral oncoproteins E6 and E7 disrupt the body’s normal defense mechanism. Namely, they inactivate tumour-suppressor proteins p53 and Rb, which under normal conditions regulate cell growth and fix DNA damage
Precancerous changes: With time, chronic infection may lead to abnormalities at the cellular level, such as cervical intraepithelial neoplasia (CIN). CIN is graded from 1 (slight changes) to 3 (extensive dysplasia). CIN3 carries the highest risk and can progress to invasive cancer if untreated.
This is why the relationship between HPV and cervical cancer is so strong and why early diagnosis is critical.
High-Risk HPV Types to Be Aware Of
While there are numerous types of HPV, fewer are closely associated with cancer. The most significant are
- HPV 16 and 18: Combined, these two strains cause approximately 70% of cervical cancers globally.
- Other high-risk types of note are HPV 31, 33, 45, 52, and 58.
Addressing these high-risk strains with vaccination and screening has been a game-changer in preventing causes and prevention for cervical cancer worldwide.
Who Is at Greater Risk of Persistence
All HPVs do not turn bad. Various factors heighten the risk of persistent infection and development of disease:
Immunosuppression: HIV-infected women or those receiving prolonged immunosuppressive treatment are at greater risk.
Smoking: Cigarette smoking attenuates cervical cells’ resistance to HPV infection.
Other cofactors: Prolonged use of oral contraceptives, coinfections like chlamydia, and malnutrition can make the cells more susceptible.

Identification of these risk factors enables clinicians to tailor prevention and surveillance strategies. Uncoded is working to develop genetic and molecular testing to more accurately identify women at highest risk of progression.
Symptoms of Cervical Cancer: When to Get Care
HPV and cervical cancer symptoms are one of the difficulties in that early signs rarely have any apparent warning. Regular screening is the reason why it is so crucial.
When the disease progresses, symptoms could be
- Abnormal vaginal bleeding (following intercourse, between menstrual cycles, or following menopause).
- Chronic pelvic pain or discomfort.
- Atypical vaginal discharge.
If you find any of these symptoms of cervical cancer, it is crucial to receive medical attention immediately.
Screening Saves Lives
Screening is the most effective method of preventing deaths from cervical cancer. There are two principal tests used:
- Pap test (Pap smear): Spots abnormal cells in the cervix before they become cancerous.
- HPV DNA test: Directly searches for high-risk HPV types that cause cancer.
Guidelines differ by nation, but generally:
- Women aged 21-29 need a Pap test every 3 years.
- Women aged 30-65 may have an HPV test every 5 years or co-testing with Pap + HPV every 5 years.
When abnormal results are detected, follow-up may comprise colposcopy and treatment of abnormal precancerous lesions (CIN) to prevent cancer development.
Also Read: Top 7 HPV and STI Symptoms Indian Men and Women Ignore
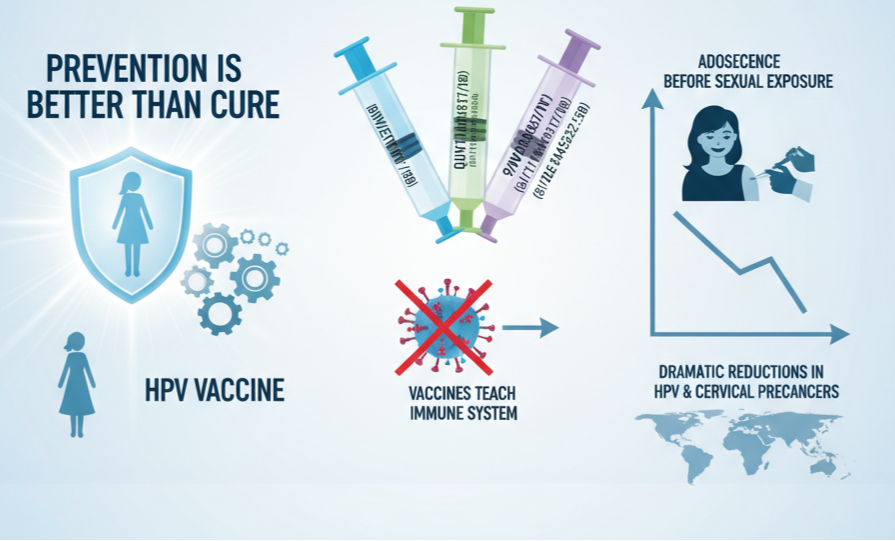
HPV Vaccination: Prevention First
Prevention is better than cure, and the HPV vaccine is one of the greatest medical breakthroughs in women’s health.
Vaccines work by teaching the immune system to identify and prevent infection from the most lethal HPV types.
The bivalent vaccine attacks HPV 16/18, the quadrivalent covers HPV 6/11/16/18, and the 9-valent vaccine protects against 9 types, including 16, 18, 31, 33, 45, 52, and 58.
Vaccination is best done before sexual exposure, preferably in adolescence.
Real-world experience demonstrates dramatic reductions in rates of HPV infection and cervical precancers in nations with extensive vaccination programs.
Prevention Beyond Vaccines
Although vaccination is important, it does not supplant other preventive measures:
- Safer sex behaviours like regular condom use can decrease, if not eliminate, HPV transmission.
- Quitting smoking decreases persistence risk.
- Adherence to regular screening guarantees early detection and treatment of precancerous alterations.
Combined, these efforts make a powerful shield against cervical cancer causes and prevention programs.
Myths vs Facts
Misinformation keeps women from seeking prevention or screening. Let’s set the record straight:
Myth: Infection with HPV always causes cancer.
Fact: Infections usually go away by themselves; only recurring high-risk HPV is dangerous.
Myth: Only promiscuous individuals contract HPV.
Fact: HPV is very prevalent and can infect anyone who is sexually active.
Dispelling these myths inspires additional women to participate in vaccination and screening programs.
Final words
Cervical cancer is preventable, but it is one of the leading causes of mortality, particularly in areas that lack access to vaccines and screening.
The World Health Organization indicates about 94% of cervical cancer deaths occur in low‑ and middle‑income countries.
This is why access to HPV vaccination and ongoing screening is so important. Organizations, governments, and diagnostic firms such as Uncoded have a significant role to play in making cutting-edge testing and preventive services more widely available, closing the gap and bridging the gap towards global elimination goals.