Blood diseases like acute myeloid leukemia (AML), myelodysplastic syndromes (MDS), chronic myelomonocytic leukemia (CMML), and inherited bleeding disorders influence the development and work of blood cells.
If left undetected and untreated, they are fatal. Traditionally, diagnosis has depended greatly on symptoms, morphology, and cytogenetics. The discovery of DNA genetic testing and next-generation sequencing (NGS) has entirely revolutionized how we diagnose, classify, and follow up on these disorders.
Now, targeted DNA/NGS testing delivers profound genetic information, finding clinically relevant variants at an early stage. This allows for quick, individualized treatment options, enabling physicians to step in before the disease advances or recurs.
Here we will discuss in detail how DNA testing will help in detecting any blood disorders. So, stay with us in the complete article.
Table of Contents
ToggleWhat “Early” Means in Blood Disorders
In the case of blood cancers and associated disorders, “early” isn’t just about detecting the disease at the onset of symptoms. Rather, it involves early application of sophisticated genetic profiling at the initial presentation.
In this manner, patients can be given the correct diagnosis and treatment plan without waiting for the disease to progress.
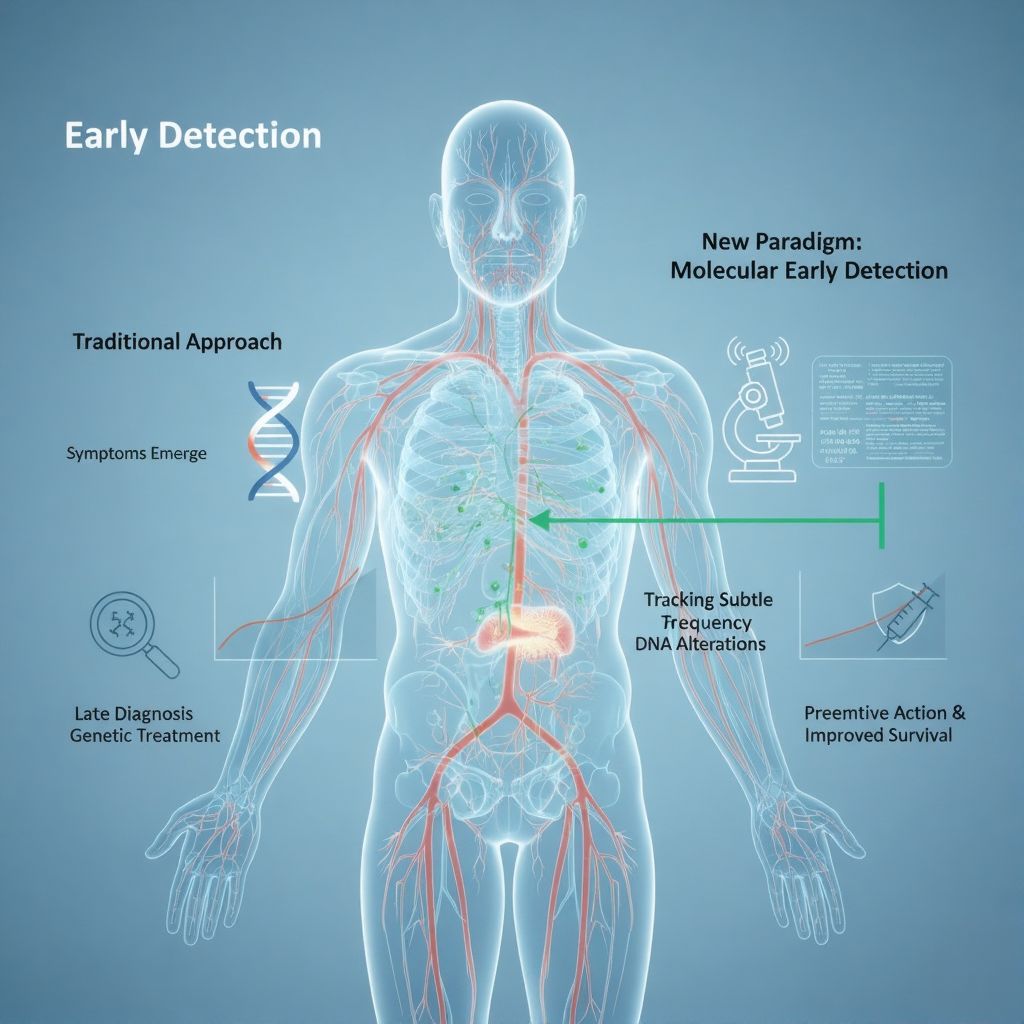
Early detection also means detection of low-frequency clones that may indicate residual disease after treatment or signify the risk of relapse.
By tracking such subtle alterations in a patient’s DNA, doctors can act preemptively, instead of waiting for complete relapse to manifest.
This paradigmic shift towards early detection on a molecular level is revolutionizing patient survival rates.
How DNA/NGS Testing Works?
In contrast to traditional approaches that screen a single gene at a time, NGS panels screen numerous genes at once with high depth of coverage, which renders them very sensitive. The tests can be performed on blood or bone marrow samples and produce an exhaustive genetic profile in a single run.
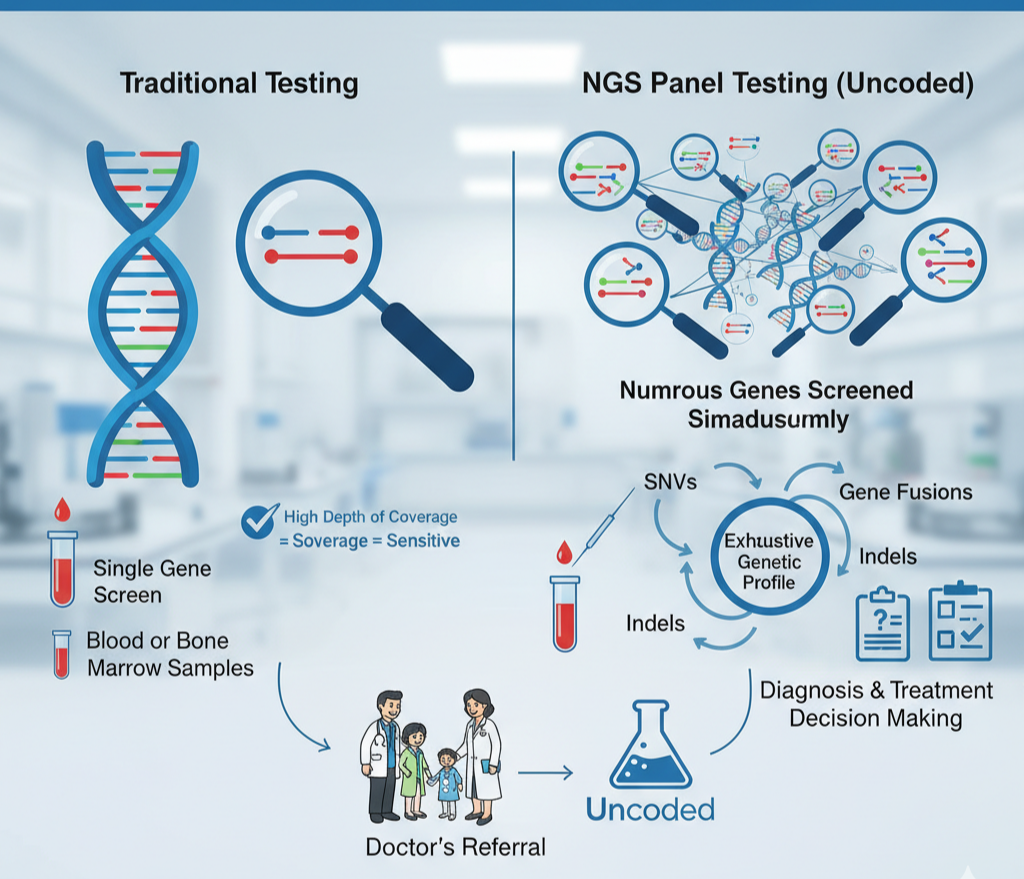
Specialty hematology-focused panels capture single nucleotide variants (SNVs), insertions and deletions (indels), and gene fusions of clinical importance. These assist not just in diagnosis but also in treatment decision-making.
For patients and families who are curious as to how to find out if DNA tests are available, the process typically starts with a doctor’s referral, and subsequently, the correct genetic test is prescribed.
In laboratories such as Uncoded, the hematology-specific DNA panels are crafted to provide sensitivity and completeness, so no critical mutation will be lost.
Key Genes of Interest in Hematologic Disorders
Various blood diseases are linked to various genetic alterations. Some of the most important targets are:
- Myeloid rearrangements and fusions like RUNX1-RUNX1T1, CBFB-MYH11, PML-RARA, and BCR-ABL1. These fusions tend to determine the leukemia subtype and direct particular treatment strategies.
- Driver mutations including FLT3, IDH1/2, NPM1, DNMT3A, and TP53. These mutations direct prognosis, assist in risk category classification, and dictate whether a targeted therapy can be used.
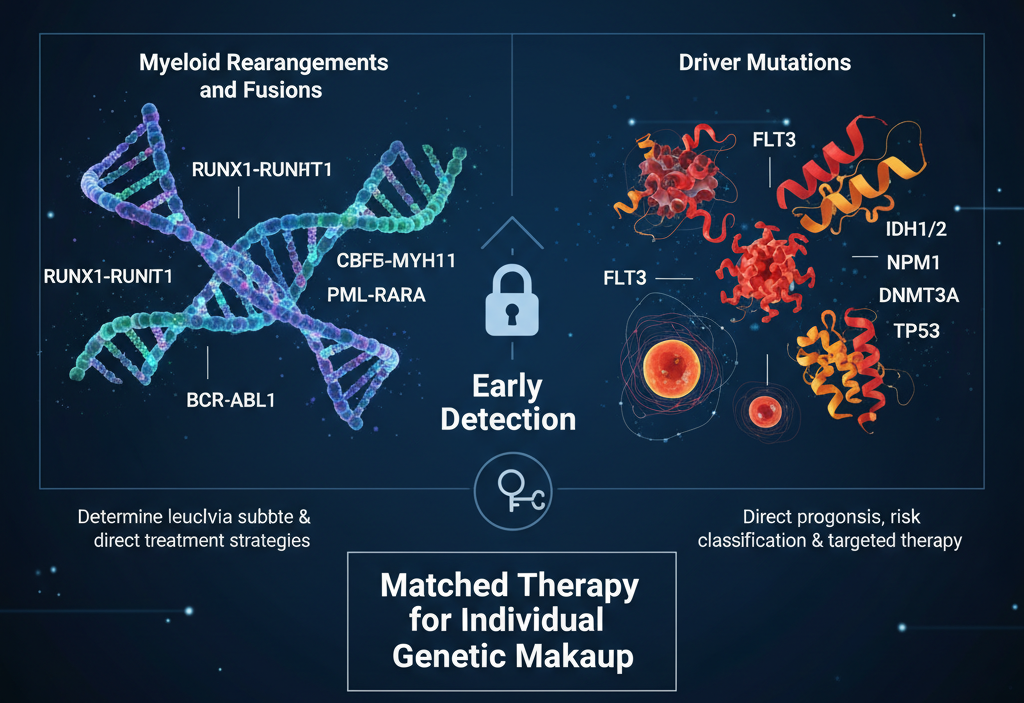
Through early detection of these genetic markers, patients are guaranteed to get matched therapy for their individual genetic makeup.
Why NGS Outcompetes Sequential Single-Gene Testing
Before, testing was carried out using a sequential single-gene approach, which meant one gene at a time. Not only did this take time, but it also meant that crucial mutations had a higher likelihood of being overlooked.
Conversely, NGS provides wide-range detection in a single run. Deep coverage prevents even low allele frequency variants or instances of genetic mosaicism from being missed.
For patients questioning how to undergo a DNA test, NGS panels are now the norm because they condense multiple diagnostic steps into a single, streamlined test.
Clinical Impact: Diagnosis to Monitoring
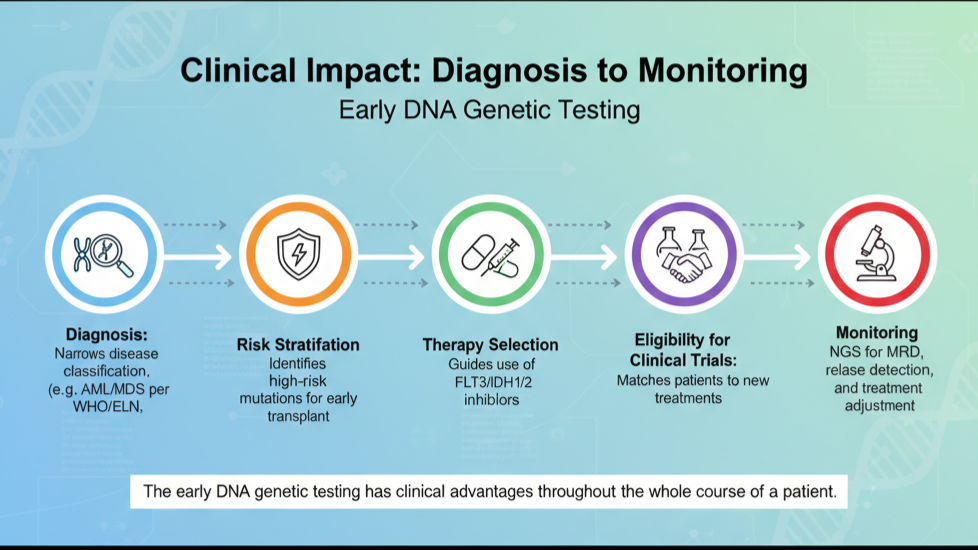
The early DNA genetic testing has clinical advantages throughout the whole course of a patient:
Diagnosis: Genetic information narrows disease classification according to WHO/ELN guidelines, particularly in the case of AML/MDS.
Risk stratification: Some mutations put patients into the high-risk category, determining whether an early transplant is required.
Therapy selection: As an example, FLT3 inhibitors or IDH1/2 inhibitors may be used when mutations are detected.
Eligibility for clinical trials: Patients can be matched to new treatments on the basis of their genetic makeup.
Monitoring: NGS enables monitoring for minimal residual disease (MRD) to identify relapse early and fine-tune treatment in response.
Role of Advanced DNA Panels in Clinical Practice
Contemporary hematology doesn’t just need to find mutations; it needs a comprehensive genetic image that directly affects the choice of treatment. Advanced DNA panels now play the cornerstone role of this method by offering depth, breadth, and clinical interpretation within a single test.
At Uncoded, the panels are specifically optimized for myeloid disorders so that all key coding areas are addressed and clinically relevant fusions are identified.
Through the incorporation of complementary RNA fusion testing, it is ensured that no rearrangement goes undetected, which is especially important for accurate classification and choice of therapy.
Let’s understand the limits and more things about DNA tests.
Quality, Limits, and Counseling
Although NGS testing is strong, it has limitations. Not all variants are identifiable, and some can be variants of uncertain significance (VUS) that necessitate follow-up. Additionally, implications of results can extend to family members, so genetic counseling is valuable.
Clinically certified panels and uniform reporting templates, like those adopted by Uncoded, provide consistency and reproducibility of results, reducing ambiguity for physicians and patients alike.
Getting Started
For families and patients interested in performing a DNA test, the process is simple:
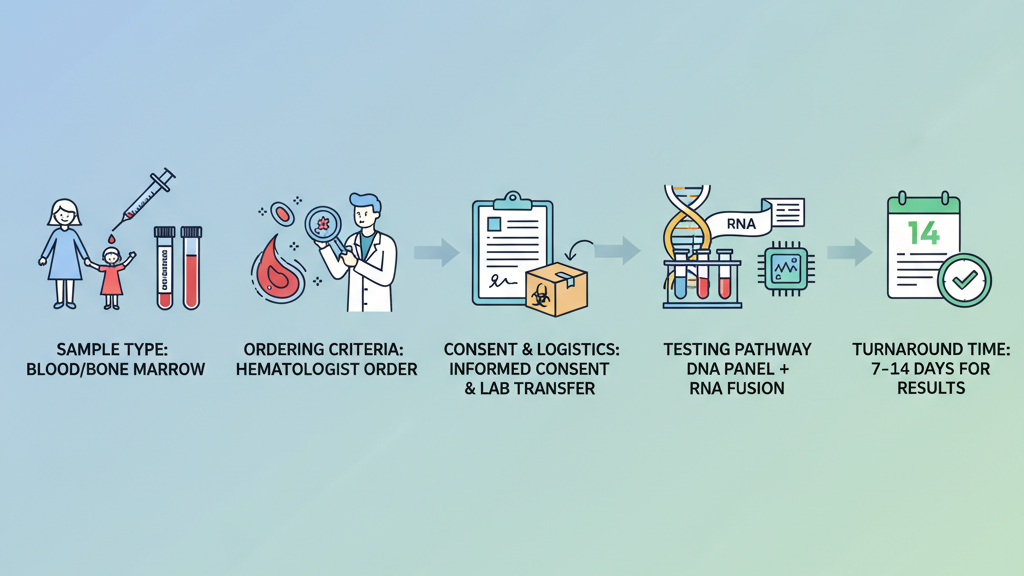
Sample type: Blood or bone marrow, as indicated by the clinical situation.
Ordering criteria: Typically ordered by a hematologist when a blood condition is suspected.
Consent and logistics: Informed consent is obtained, and the sample is forwarded to a reference lab.
Testing pathway: DNA panel testing can be combined with RNA fusion testing for completeness.
Turnaround time: Results are typically available within 7 to 14 days, allowing timely planning of treatment.
Knowledge of this pathway makes the patient feel more ready and comfortable with the process.
To Wrap Up
Time is of the essence in blood disorders. Early, panel-based DNA genetic testing shortens the timeframe to correct diagnosis, enhances treatment targeting, and optimizes long-term tracking.
By identifying mutations and fusions early on, NGS allows physicians to transition from suspicion to action rapidly, providing patients with their best hope for good outcomes.
With Uncoded solutions, Indian patients are able to receive cheap, effective, and complete DNA testing specifically for hematologic disorders.
For those seeking to know how to inquire about DNA test availability or how to undergo a DNA test, the solution is to visit a specialist who can advise on testing at the appropriate stage.
Finally, DNA testing is no longer an add-on diagnosis—it is the platform on which current care for blood disorders is built, offering precision, expediency, and promise to patients everywhere.

